When will I make decisions?
- You will be asked to make healthcare decisions ONLY when the person is no longer capable of making a healthcare decision for him/herself. (See the section on Capacity to learn more.)
- When the person is incapable of making a healthcare decision a
healthcare provider will ask you to provide consent for a decision.
- Your role is to make decisions the way the person would have made them for themselves.
Some examples of these times where you might be asked to make decisions include:
If the person becomes capable, they will again make their own healthcare decisions.
To learn more about what mental capacity means and how it is assessed click here.
Priya and Jacob
- Neither Priya nor Jacob have the capacity to make all of their own healthcare choices.
- However there may be some decisions they are capable of making for themselves.
- Even when they are incapable, both Priya and Jacob should be included in the decision-making process as much as possible.
- Read their stories below to see what the role of their SDM would be in ACP and decision-making.
Priya is 84 and has dementia. She has been living in a Long-term-care facility for 4 years.
She has been admitted to hospital a few times for pneumonia.
Her SDMs are her three children.
Her SDM's will share decision-making when she requires transfer to hospital or treatment of her pneumonia.
Their role in ACP will be to learn about dementia and what they might expect to happen in the future.
Jacob is 9 years old. He was diagnosed with Leukemia when he was 4.
His parents had been making all of his healthcare decisions as his SDMs.
Jacob is now starting to learn and understand about his own illness.
For decisions where Jacob is not capable, his parent will continue to make healthcare decisions. But Jacob should be involved as much as he can be.
ACP for Jacob and his parents will include a discussion of what to expect in the future. Even if Jacob is not capable, his wishes, thoughts and feelings are an important part of ACP conversations.
What is my role if the person is still capable?
-
If the person is still capable, your role will be supportive.
- It can be very helpful for you to attend medical appointments (with their permission), to listen to the health information that is being provided and to ask questions.
- When the person is capable, you will want to talk with them to understand their values, beliefs, and what is important to them.
- Your role in the ACP process is to learn as much as you can about the person and their illness to make the best decision for them if you ever have to.
Althea is healthy and capable. Her SDM's role would be to learn about her values and what is important to her.
While Althea is capable, it is a chance for her SDM to ask her questions about any wishes she may have for her future healthcare needs.
Bob is capable but he has some issues with his heart. In addition to learning what is important to Bob, his SDMs also need to start learning about his heart issues and what to expect in the future.
At Bob's request, his SDMs may also play a supportive role in decision-making at any time.
Tran's SDM is her husband. His role as an SDM will be to learn about both her values and what they may expect to happen in the future with her breast cancer.
Even though Tran is capable of making her own decisions, her SDM and her family are vital supports on her cancer journey.
How does an SDM make healthcare decisions?
- Making healthcare decisions for other people can be challenging, especially when you have to do this during difficult times.
The person you have to make decisions for might be someone very close to you. It could be someone you care a lot about and want to look after.
- It might help to know that there are rules that give you instructions on how to make these decisions.
You must consider the person’s:
- Prior Capable Wishes
- Best Interests
- You first look for capable wishes. If there are none that apply or they are impossible to follow, then you use best interests to make a decision.
- If the person has had an advance care planning conversation, you may have discussed some of their prior capable wishes. You may also have discussed their values and beliefs that will help you think about best interests in the current situation.
- If the person is still capable and you are preparing for your future role as an SDM, now is a good time to talk about their values, beliefs, and wishes.
- The person can help you understand how you should make decisions for them in the future, based on their values and beliefs.
Guidance on Prior Capable Wishes
- Think of anything the person may have said that applies to the decision you have to make.
- It could have been something they said, wrote down, or recorded on a video.
- Which is the most recent? This is the one you need to consider, even if it’s not written down.
- It is your role as an SDM to decide if the wishes apply to decision you are being asked to make.
- It is also your role to decide what the wish means. ACP conversations are a great time to ask the person to explain what a wish means.
A Person's Best Interests
When the healthcare team suggests a treatment or plan, your role is to think about these questions:
- Will the treatment or plan:
- Improve the current condition or well-being?
- Prevent worsening of the current condition or well-being?
- Slow down the process of getting worse?
- Will the person get better, worse or stay the same if the treatment or plan is not followed?
- Do the benefits outweigh the risks of harm? (**risks/benefits as the person would see them)
- Is there a less aggressive option that might help the person just as much?
Frequently Asked Questions
How will my SDM make decisions if I have not had any ACP conversations?
- If your wishes are not known, your SDM(s) must act in your “best interests.”
- “Best interests” has a specific meaning in law: your SDM must consider a person's values and beliefs.
- They would also consider:
- Your health condition
- If you are likely to improve, remain the same or deteriorate without the treatment
- The risks and benefits of the treatment options
Should I include my SDM in ACP conversations?
- It is good idea to involve your SDM as much as possible in these conversations.
- ACP is meant to prepare your SDM to make your healthcare decisions in the future if you loses capacity to make your own decisions.
- If you are not comfortable including your SDM in ACP conversations, think if there is someone else you would prefer in the role.
- Your SDM may have to make some hard choices. Knowing about the person and their values can make this easier.
Who Determines Mental Capacity?
- The health care provider proposing the treatment will determine if you are mentally capable of consenting to or refusing treatment.
- For example, if you are having surgery, it will be your surgeon who determines if you are capable of agreeing to the surgery.
- If you are found incapable, you have the right to ask the Consent and Capacity Board to review that finding. The health care provider who believes you are mentally incapable must tell you about that right of review.
What kind of decisions might an SDM make on my behalf?
If you cannot speak for yourself, your SDM(s) will make decisions for your care. These decisions will be based on the conversations you already had about your wishes, values and beliefs. These decisions could include things like whether or not to:
- have tests, surgery or other medical care
- stop or start a treatment
- move to a long-term care home
Can an automatic SDM choose not to make my healthcare decisions?
Yes. Any SDM can choose not to make your healthcare decision. If this happens, your healthcare provider will ask the next person lower down on the hierarchy list to make your healthcare decision.
Does my SDM have to follow my wishes?
- Your SDM must look at any wishes you made when you were mentally capable.
- Your SDM must ask themselves two questions:
1) Do they apply to the current decision?
2) Are they possible to follow?
- SDMs do not have to follow a wish that is impossible to honour.
- There are many things that can make a wish impossible to honour. Decisions will depend on the person's health and care needs, finances and the number of people around who can help care for a person.
- For example, a person may tell an SDM that they wish to remain at home but there may be times when a hospital or long-term care
is the best place to receive care based on the person's needs.
What if more than one person is at the same level on the SDM hierarchy?
- Looking at the list of people who can make decisions, a person may have more than one person at the same level (e.g children or siblings)
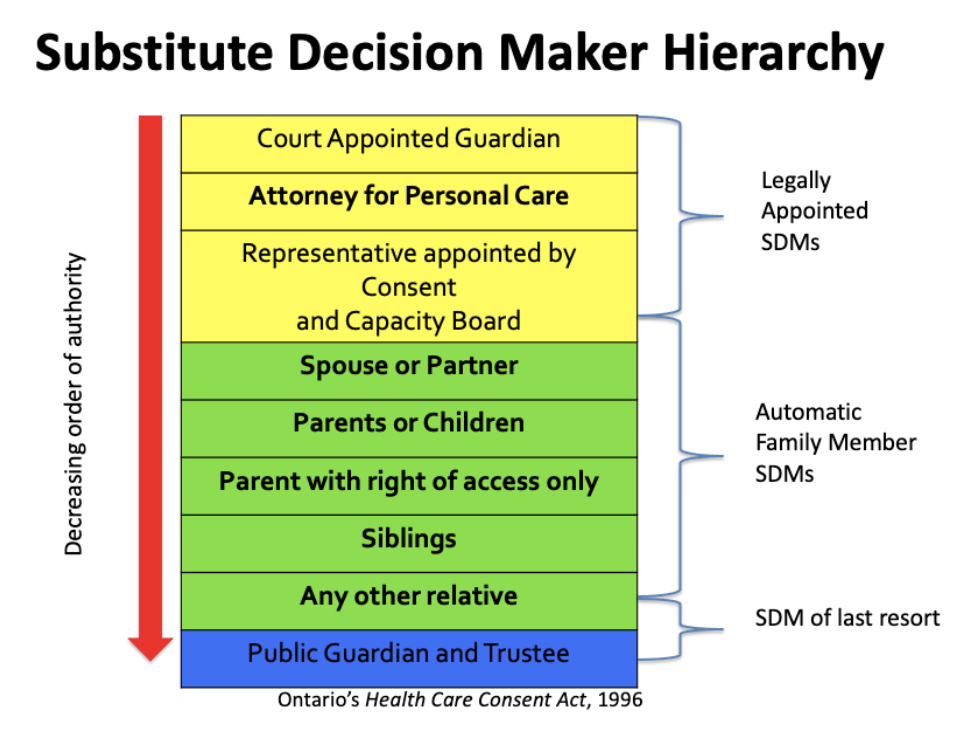
- If they are highest on the list, they would automatically make decisions. They must make decisions together (jointly) or decide among themselves which one will act as your SDM.
- For example, if a person has three children (#5 on the list), all three are entitled to act as SDM(s). They must act jointly and agree on any decisions for a person's health care or they can agree that only one of them will make decisions. The health professionals cannot pick which one of the three should make decisions. The three children must decide among themselves whether they will all act together or if only one of them will.
What if SDM(s) disagree amongst themselves?
If people who are equally entitled to act as SDM(s) cannot agree on the decisions about your treatment, you may have several options depending on your clinical setting:
- Make sure you have explored the underlying illness understanding and underlying reasons behind the disagreement as there may misunderstandings that are leading to the issue.
- If you have access to bioethics consultation, they may be able to support the SDM(s) to reach consensus.
- If you cannot reach agreement among the SDM(s), the Public Guardian and Trustee is required to act as SDM. The Public Guardian and Trustee does not choose between the disagreeing decision-makers but makes the decision instead.